Your virtual assessments are better than our previous in-person assessments.
The Helper Bees’ experienced nurse assessors, both in-house and contracted, use our HIPAA-compliant digital assessment tool to conduct long-term care assessments in person, virtually, or telephonically. This results in a 30% cost savings for virtual assessments and 0% infection risk.
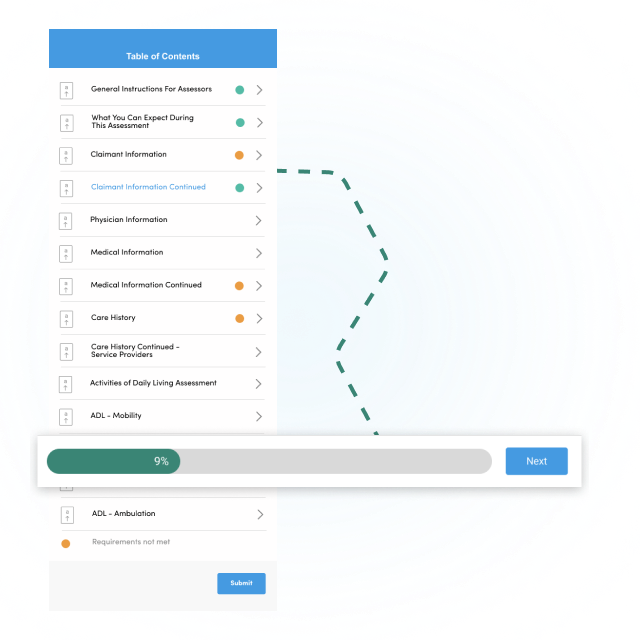
The digital Benefit Eligibility Assessment allows The Helper Bees’ nurses to quickly adapt while gathering accurate data from the insured, family, or caregiver. Our digital assessment transforms the standard, meticulous, paper-based documentation into an easy-to-navigate intelligent form.
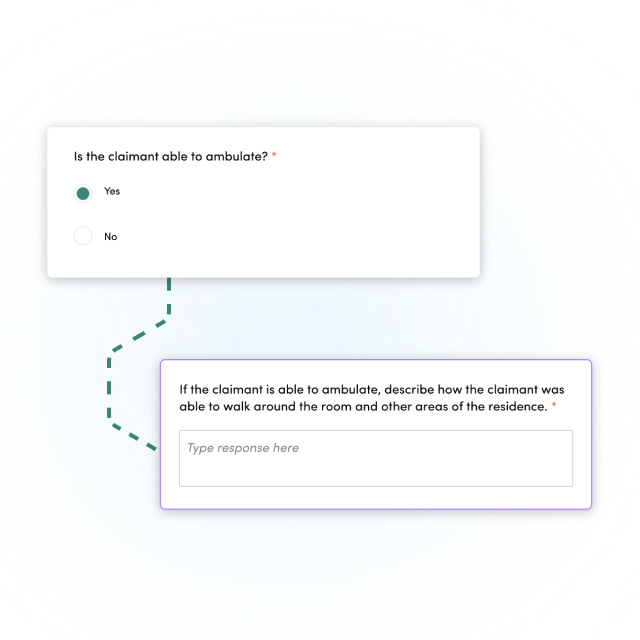
The Helper Bees’ virtual assessments allow for the gathering of accurate information on a home care recipient with minimized risk of infection transmission for both clinician and insured. It quickly responds and adapts to changing scenarios and can make real-time updates that help to improve the nimbleness and relevance of the data gathered.

We handle the complete benefit eligibility process including medical record retrieval, plan of care and chronic illness certification creation, and caregiver assessments. Seamless workflow integration, unprecedented data analytics, and automation capabilities save insurers time and money.
Your virtual assessments are better than our previous in-person assessments.
Top 3 Largest LTC Claims Block