Shaving off the excess billing is where we see ROI. We also achieve customer satisfaction, efficiency gains, and save on processing and data entry with the digital invoicing.
The Helper Bees Digital Invoicing solutions simplify claims submission, improve data collection, and help detect fraud using advanced analytics. Our home care electronic visit verification (EVV) solution uniquely leverages continuous GPS data to track the entire visit – not just the beginning and end. Proven cost savings compared to paper = 18% with 5x ROI for Facility Digital Invoicing.
Our industry-leading fraud analytics dashboard is accessible 24/7 and has been used by some of the largest long-term care insurance providers to complete surveillance and reduce fraud. The dashboard utilizes data collected from the home to stratify and score risk, allowing insurers to make informed decisions. Alerts are triggered by suspicious activities from home care claims and non-billable items from facility claims.
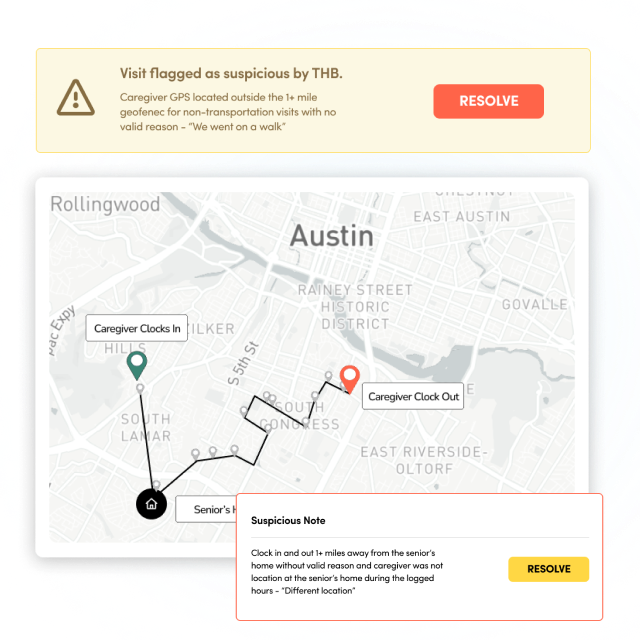
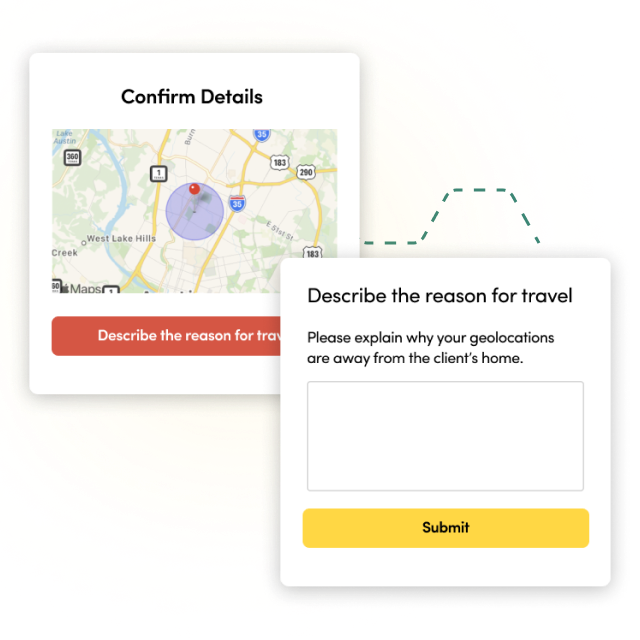
Our home care Electronic Visit Verification (EVV) solution leverages continuous GPS data, which enables an additional layer of fraud protection and ultimately reduces carrier costs.
For our carrier partners, the home-based solution has reduced soft fraud by 18% per visit, reduced invoices not in good order (NIGO) to 0%, reduced duplicate invoices by 50%, and doubled the number of claims closed due to inactivity.